FLEX Vessel Prep system data (3 studies) was presented at LINC 2021 (Leipzig Interventional Course) in Germany.
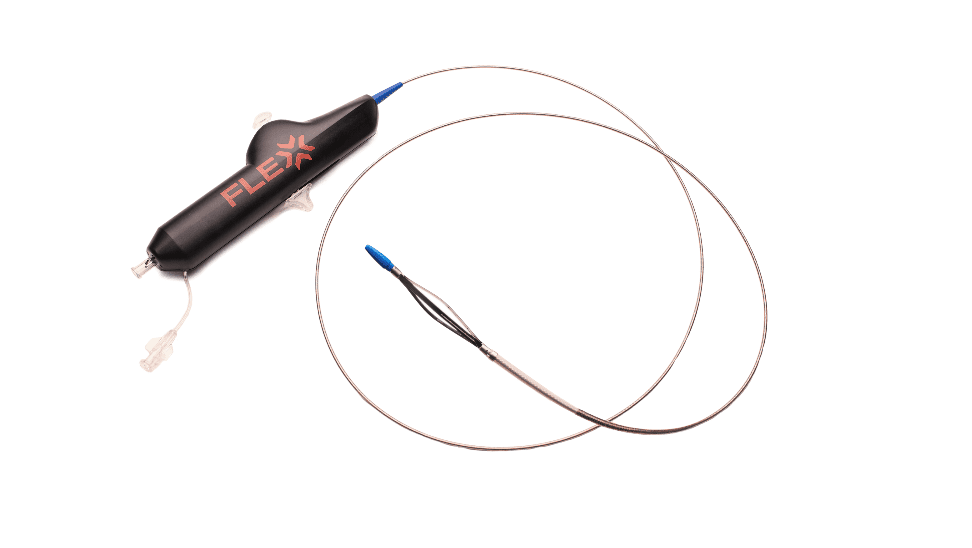
VentureMed develops and markets innovative endovascular devices that address unmet needs in the treatment of peripheral arterial disease (PAD) and stenoses of arteriovenous (AV) fistulas and grafts. Its FLEX Vessel Prep System is designed to modify plaque and prepare vessels with complex femoropopliteal arterial disease, including in-stent restenotic (ISR) lesions, prior to delivery of the definitive therapy.
“Individually and collectively, these three studies report compelling data,” said J. Robert Paulson, Jr., president and chief executive officer of VentureMed. “The data demonstrate that longitudinal, circumferential micro-incisions delivered by the FLEX Vessel Prep System safely and consistently modify plaque to improve vessel compliance and increase luminal gain, with minimal trauma to the vessel, which may reduce the need for stenting and facilitate the delivery of drug therapies into the vessel wall. The FLEX Vessel Prep System allows physicians to modify plaque and prepare diseased vessels of any length to optimize their choice of definitive revascularization therapy.”
The following are summaries of the three studies presented at LINC 2021, which features state-of-the-art lectures from leading interventional centers:
12-Month Results of Micro-Incision Vessel Prep System Showing Acute and Long-Term Benefit in Superficial Femoral and Popliteal Arteries
(Dr. Thomas Zeller, Ph.D., University Heart Center Freiburg – Bad Krozingen, Germany; Dr. Daniel Périard, et al., HFR-Hôpital Cantonal Fribourg, Switzerland)
This single center study assessed the impact of vessel preparation with FLEX VP longitudinal, controlled-depth, micro-incisions prior to drug-coated angioplasty balloon (DCB) or percutaneous transluminal angioplasty (PTA) therapy, acutely, and at 6- and 12-months.
Study findings:
- Sixty-three patients with moderate-to-severe symptomatic femoropopliteal PAD, with lesions averaging approximately 200 mm in length, were treated with the FLEX VP to create circumferential, controlled-depth micro-incisions prior to delivery of the definitive DCB (paclitaxel) or PTA therapy.
- The freedom from target lesion revascularization (FTLR) at 6- and 12-months was 98.5% and 93.7%, respectively with a low provisional stent rate of only 16.9%.
Patterns and Number of Dissections with Atherectomy versus FLEX VP: an IVUS Assessment (Dr. Nicolas W. Shammas, M.S., et al., Genesis Health System, Davenport, Iowa, United States)
This single-center, comparative, prospective study was based on published data demonstrating that dissection, not plaque compression, is what opens the lumen of obstructed vessels post-PTA. Published clinical data also has demonstrated that severe dissections per NHLBI classifications (Type C and higher) and dissections involving the adventitia are likely to be associated with worse outcomes after definitive PTA therapy. This study evaluated the differences in dissections between atherectomy and the FLEX VP system in femoropopliteal arteries and included de novo and restenotic lesions using intravascular ultrasound.
Study findings:
- In lesions with comparable treatment lengths and presence of calcium, there was a pattern of significantly fewer and less severe dissections after FLEX VP vessel preparation as compared to atherectomy.
- There were no differences in the extent of new dissections following delivery of the definitive PTA therapy.
- This data suggests that FLEX VP may be less traumatic as vessel preparation.
Lesion Modification with a Micro-Incision Vessel Preparation System Enhances Balloon-Based Drug Delivery in Complex Porcine Restenotic Lesions
(Rami Tzafriri, Ph.D., et al., CBSET, Boston, Mass. The United States)
This study examined if and how a vessel preparation system delivering micro-incisions could enhance in vivo paclitaxel (delivered from a DCB) retention in a complex porcine ISR lesion model design. Optical coherence tomography (OCT) images of the baseline ISR images confirmed barriers to delivery of DCB therapy. The animals were either (a) imaged by OCT and treated with a DCB and then re-imaged, or (b) imaged by OCT, re-imaged after micro-incisions were delivered by the FLEX VP System, treated with DCB and then re-imaged again. The animals were survived to 1, 15 or 30 days and the treated arteries then were processed to measure retention of paclitaxel concentrations.
Study findings:
- OCT imaging of ISRLs revealed smooth stenotic surfaces posing significant barriers to penetration as evidenced by remarkably low paclitaxel concentrations at 1 day in standard vessels (<0.9 ng/mL).
- OCT imaging of the lesions treated with the FLEX VP System demonstrated atraumatic micro-incisions along the length and circumference of the vessels, with no dissections, and enhanced tissue retention of paclitaxel as compared to the vessels treated with DCB alone.