At a Glance:
- New weight loss medications are impacting bariatric surgery practices
- Surgeons are adapting to changes in patient volume and treatment options
- Advancements in surgical techniques are improving patient outcomes
- Accessibility and affordability of treatments remain significant challenges
- A comprehensive approach to obesity treatment is crucial for patient success
The field of bariatric medicine is experiencing significant shifts due to innovative medications and surgical techniques. Dr. Monique Hassan, MD, FACS, FASMBS, DABOM, a board-certified bariatric surgeon, speaks with Surgery Unified, maker of SurgeOn, the app revolutionizing the surgical world with digital collaboration and online resources. They discuss the latest trends, challenges, and advancements in obesity treatment. Their conversation covers the impact of new weight loss drugs, cutting-edge robotic surgical procedures, and the future of bariatric care.
SurgeOn: Dr. Hassan, can you tell us about the recent changes you’ve observed in your practice, particularly regarding new anti-obesity medications?
Dr. Hassan: We’ve seen a significant impact from medications like Ozempic and Mounjaro. There’s been a two-fold effect: an increase in patients interested in medical weight loss, and a hesitation from some patients to proceed with surgery as they want to try medication first. As someone board-certified in obesity medicine, I can still see these patients and help manage their obesity through various approaches.
SurgeOn: How has this affected your surgical volume?
Dr. Hassan: We’ve seen a dip in surgical volume over the last six months. Previously, I would typically perform four cases a day. Recently, there have been days with no cases at all. While we’ve had some cancellations due to COVID-19, the impact hasn’t been as significant as the shift towards medication options.
Can you elaborate on the pros and cons of these new medications?
The positive aspect is that these medications are normalizing discussions about obesity and providing another treatment option. Unlike older drugs such as phentermine or contrave, which had limited success, these new medications are showing promising results. However, the major drawback is their [high] cost…
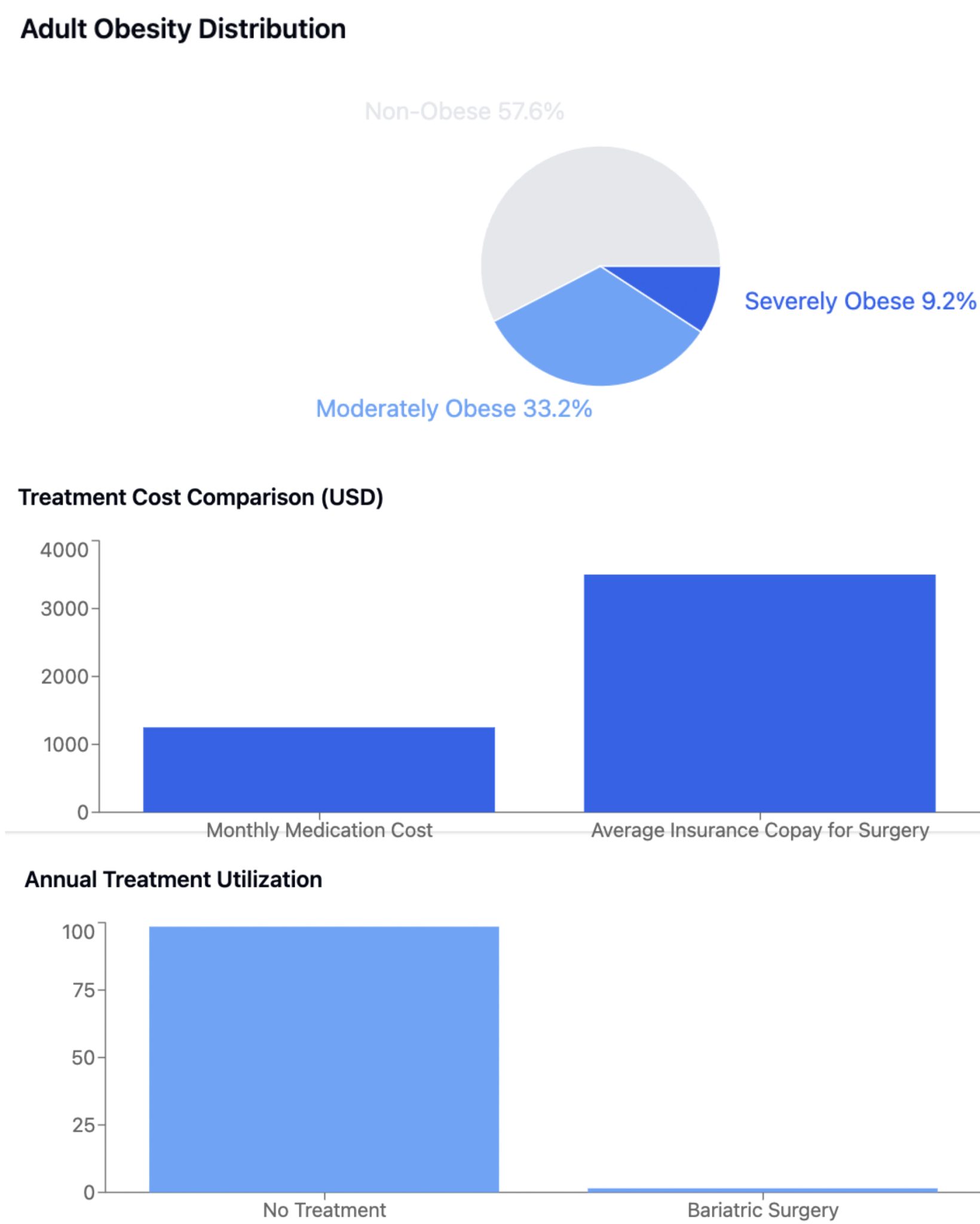
Recent studies have shown that approximately 42.4% of American adults are considered obese (BMI ≥ 30). Of these, about 9.2% fall into the severe obesity category (BMI ≥ 40). However, it’s estimated that only 1-2% of eligible patients undergo bariatric surgery each year, highlighting a significant gap in treatment utilization. Patients using new weight loss medications, such as Mounjaro, can lose approximately 20% of their excess body weight. However, with costs ranging from $1,000 to $1,500 per month, accessibility remains a significant barrier for many patients. This price point contrasts sharply with the potential long-term cost-effectiveness of bariatric surgery, which is often covered by insurance for eligible patients.
Let’s talk about the importance of lifestyle changes. How do you address this with patients, regardless of their treatment path?
I emphasize that both surgery and medication are adjuncts to lifestyle changes, not replacements. Patients still need to focus on a balanced diet and regular exercise. We know that 80% of weight loss is diet-related, but exercise is crucial for maintaining weight loss long-term. It’s about developing a different relationship with food and understanding that moderation is key… [and] while medications and surgery can provide significant initial weight loss, maintaining that loss requires consistent lifestyle changes. A balanced diet rich in proteins, vegetables, and whole grains helps patients feel satiated while providing essential nutrients. Regular exercise, ideally a combination of cardio and strength training, not only burns calories but also improves metabolism, mood, and overall health. We encourage patients to find activities they enjoy to make exercise a sustainable part of their routine.
What can you tell us about the advancements in bariatric surgery techniques?
We’ve made significant strides in surgical techniques. I now perform 100% robotic surgery, which is a far cry from the open procedures of the past. Patients are often going home the same day, even after complex procedures like gastric bypass. We’ve also refined our approach to post-operative care, including simplified vitamin regimens. One exciting development is the increased adoption of procedures like the duodenal switch and single anastomosis duodenal switch. These offer maximum weight loss potential and excellent diabetes control for patients with higher BMIs. [But] the duodenal switch is a complex procedure that combines a sleeve gastrectomy with an intestinal bypass. It’s particularly effective for patients with very high BMIs or severe diabetes. The single anastomosis duodenal switch, also known as SADI-S, is a simplified version that maintains most of the benefits while reducing surgical complexity and potential complications. Both procedures can lead to significant long-term weight loss and dramatic improvement in obesity-related health conditions.
How do you stay current with these advancements?
Staying connected with colleagues is crucial. I’m a moderator on SurgeOn and participate in various professional Facebook groups. I’m also on the Executive Council for ASMBS, our national society for bariatric surgery. Recently, I attended the IFSO 2024 conference in Australia, which provided valuable insights into global approaches to obesity treatment.
Looking ahead, what trends do you see shaping the future of bariatric care?
The COVID-19 pandemic has accelerated the shift towards home-based care and remote monitoring. We’re seeing more interest in wearable devices for continuous health tracking. There’s also a growing focus on sustainability, with a move away from single-use devices where possible. These trends are likely to continue shaping our field in the coming years.
Can you elaborate on how wearable devices are impacting bariatric care?
Wearable devices are revolutionizing how we monitor patients post-operatively and during medical weight loss treatments. These devices can track physical activity, sleep patterns, and even some vital signs. This continuous data allows us to intervene earlier if we notice concerning trends and to provide more personalized advice to patients. Some advanced wearables can even monitor glucose levels continuously, which is particularly beneficial for our diabetic patients.
What advice would you give to young professionals entering the field of bariatric medicine?
I’d encourage them always to consider the end user – the patient – in everything they do. Empathy and understanding are crucial in this field. It’s also important to adopt a design thinking approach, considering multiple possibilities and innovative solutions. The field of bariatric medicine is constantly evolving, and staying open to new ideas is key to providing the best possible care for our patients.
Bariatric medicine is at a crossroads, with practitioners like Dr. Hassan balancing innovative medications, surgical interventions, and wearable tools. The challenge lies in providing personalized, accessible care while navigating the complexities of insurance coverage and rapidly advancing technologies. By maintaining a patient-centered approach and embracing new developments, the future of obesity treatment offers hope for improved outcomes and quality of life for those struggling with weight-related health issues. As the landscape continues to change, the integration of medical, surgical, and lifestyle interventions will be crucial in addressing the global obesity
Monique Hassan, MD, FACS, FASMBS, DABOM
Assistant Professor Of Surgery, Texas A&M University
Assistant Professor Of Surgery, Baylor College of Medicine
Minimally Invasive and Bariatric Surgeon, Baylor Scott & White Health
About Surgery Unified
Despite continual medical and technological advances, the surgical world was at a standstill. Antiquated ways of sharing best practices, exploring new technology, and building meaningful relationships with colleagues were the norm. We had first to reimagine and then thoroughly reinvent the surgical world to bring it all together in a new way. Surgery Unified is a privately held company focused on reinventing the surgical world. We started a larger conversation to bring more people together and align on the mission-critical initiatives.
About the Author: Dr. Jeremy Heffner is Chairman of Surgery at Lima Memorial Health System, Co-founder and COO of Surgery Unified. He was a bioengineer with GE Medical Systems and the NIH. He is board-certified in General Surgery and Surgical Critical Care and completed his fellowship training in trauma surgery at the University of Michigan. He has received national research awards from the American Hernia Society and the Eastern Association for the Surgery of Trauma.
About SurgeOn The SurgeOn app is a built-for-purpose community and learning app built by surgeons for surgeons. With over 13,000 vetted U.S. surgeons as users, this app redefines collaboration, knowledge sharing, and skill enhancement and has reinvented the world of surgical collaboration. Private communities, cutting-edge video sharing, and a comprehensive surgical procedure library empower exploration, discovery, learning, and connection in a community tailored to surgical expertise. SurgeOn maximizes professional potential through the power of one app. Visit https://home.surgeonapp.com/ to learn more.
