Hospital-acquired infections (HAIs) have been an ongoing concern for healthcare systems for decades. A patient who enters a hospital can acquire an infection as soon as 48 hours into their stay. According to the Center for Disease Control and Prevention (CDC), on any given day, it’s an estimated 5% or 1 in 31 hospital patients contract a hospital-acquired infection while being treated in a medical facility. These infections can lead to death and high costs for hospitals. The CDC lists antimicrobial resistance as an urgent global public health threat, with related infections killing an estimated 5 million people in 2019 alone.

In addition to surface and hand sanitization as a recommended practice for infection control prevention, continuous air sanitization can further provide healthcare systems with a solution that addresses the ongoing problem of HAIs.
COVID-19’s Impact On Hospital Acquired Infections
When the COVID-19 pandemic hit in March 2020, intensive care units were forced to reorganize their systems to accommodate the influx and overflow of patients, making it extremely difficult to provide adequate care to all patients with no end in sight. There were shortages of staff protective equipment, high rates of staff sick leave, longer lengths of patient stay, and stretched ICU capacity. Given these circumstances, the healthcare system was strained, overwhelmed and vulnerable – leading to more opportunities for infection spread.
Now in a post-pandemic world, hospital occupancy rates have gone down and healthcare facilities have started to return to normalcy. Yet, hospital-acquired infections remain an issue. Harmful pathogens continue to linger in the air, remaining a threat to patients – especially those who are immunocompromised, as well as everyday healthcare workers, facility staff, and even visitors. Hospital-acquired infections can cost the hospital anywhere up to $40,000 per infection.
Most Common Hospital-Acquired Infections
There are four main categories of infections that are the most common to acquire, which are surgical-site infections, ventilator-associated pneumonia, central-line-associated bloodstream infections, and catheter-associated urinary tract infections. These four categories contribute to three-quarters of the HAIs that hospitals see on a daily basis. A few of the most common symptoms that can indicate an infection are coughing, shortness of breath, abdominal pain, and palpitations. Although hospitals can help manage minor illnesses that patients have, being in healthcare facilities inevitably puts patients at a high risk of acquiring additional illness or infection that can be very harmful. This is even more prevalent in ICU patients. According to a study with 231,459 ICU patients, 19.5% of them acquired at least one HAI.
Surges of Hospital-Acquired Infections through Recent Years
Many HAI’s are caused by antibiotic-resistant (AR) bacteria. The CDC’s 2022 special report: COVID-19 U.S. Impact on Antimicrobial Resistance cites surge levels of dangerous superbugs year over year, including Acinetobacter up 78%, Candida auris up 60% and MRSA by 13%, from 2019 to 2020. These and other harmful bacterial and fungal organisms can remain in the atmosphere and on surfaces for weeks or even months – continuously contaminating spaces and infecting more people. Losing the efficacy of certain antibiotic treatments will threaten the ability to treat and manage infectious diseases and complications, especially for immunocompromised patients, thus making prevention of infection even more crucial.
Reducing Hospital-Acquired Infections with Improved Indoor Air Quality (IAQ)
The COVID-19 pandemic has raised awareness of the importance of indoor air quality (IAQ) and air sanitization – and how eliminating airborne pathogens can help prevent more infections in the long term – including ongoing HAIs.
In meeting this demand, competing air cleaning brands and technologies have surfaced, but not all devices meet medical-grade standards. Some technologies are purely air filtration technologies and do not actively eliminate harmful airborne pathogens, thus allowing the opportunity for recontamination. HVAC UV technology can eliminate some pathogens, but cannot stop close-range, real-time transmissions – the primary way airborne infections are spread. Bipolar Ionization technologies can emit harmful byproducts like ozone, and if used alone without supplemental ventilation technology, are less effective. Such devices can provide a false assurance that the indoor air is safer and being cleaned efficiently. Effective air sanitization devices use a combination of medical-grade HEPA filters to reduce airborne particulate and Ultraviolet Germicidal Irradiation (UVGI) technology to eliminate airborne pathogens, and produce sanitized air with no harmful byproducts.
Medical-Grade, FDA Cleared Air Purification Technology
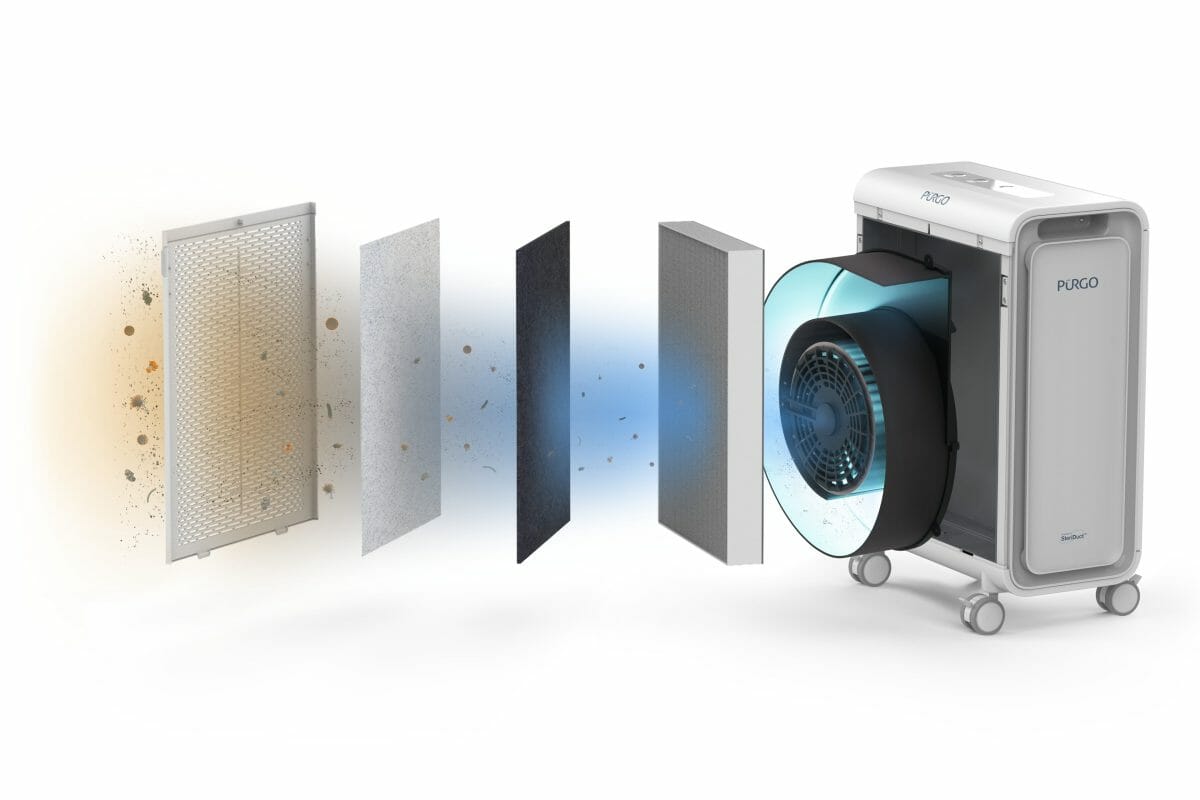
AeroClean was founded by a world-renowned orthopedic trauma surgeon, an accomplished aerospace engineer with multiple patents, and a successful entrepreneur who all came together seeking a solution to address HAIs. They developed Pūrgo™, a room air sanitization solution that is an FDA-cleared Class II Medical Device, which safely uses patented germicidal UV-C LED technology, the SteriDuct™, to eliminate 99.99% of harmful airborne microorganisms – including the MS2 bacteriophage, a surrogate pathogen for COVID-19, as well as the Omicron variant of SARS-CoV-2, which the CDC identifies as the current dominant variant in the United States.
A low-maintenance solution, Pūrgo™ requires only a simple plug-and-play installation and can be deployed in clinical areas such as the ER, treatment and surgical spaces, as well as non-clinical areas like waiting rooms, staff lounges, and lobbies – or any indoor space. Air is exchanged multiple times per hour while being actively filtered and sanitized, outputting cleaner, safer, air. When there is less particulate matter (PM) in the air, less PM settles on surfaces, requiring less surface cleaning, potentially allowing healthcare facilities to reduce overall cleaning and maintenance costs and use of harsh cleaning solutions.
What Does Improved IAQ Mean For The Future of Healthcare?
Should infection control management protocols include continuous air hygiene, improved IAQ could make significant impacts in healthcare. Paired with existing practices such as surface and hand sanitization, the prevention of more HAIs and deaths from infections could be possible, and healthcare costs would reflect these outcomes. Healthier IAQ could also help address other healthcare challenges like absenteeism and turnover.
In addition to the possible outcomes of improving IAQ in healthcare facilities alone, the recent White House Summit on Improving Indoor Air Quality gathered health and ventilation experts, private sector, and education leaders to discuss the importance of IAQ, not just as a way to prevent the spread of infectious diseases, like COVID 19, but also to create healthy workspaces and buildings for everyone. At the summit, Dr. Joseph Allen from the Harvard University T.H. Chan School of Public Health said, “Our buildings have an outsized impact on our health.” Because we spend 90% of our time indoors, he added “that the person who manages your building has more of an impact on your life than your doctor.” The new website released by the White House shares resources and urges a call to action for organizational leaders and building owners and operators of all types to assess their indoor air quality and make ventilation, air filtration, and air cleaning improvements to help keep building occupants safe.
We need to educate ourselves on how indoor air quality in our everyday environments is impacting the healthcare system and our overall health. Preventing HAIs and improving our long-term health should start before a stay or visit to the hospital.
Editor’s Note: Jason DiBona, CEO of AeroClean (Nasdaq: AERC), is leading the charge to keep businesses running and people connecting – safely. AeroClean’s seasoned executive team, engineers, doctors, and scientists have developed proprietary, proven, patented technology and products that provide continuous air sanitization to control pathogen risks and keep our hospitals, offices, schools, and businesses safe.
Jason brings more than 25 years of experience in developing and executing strategies for sustainable growth. He has held leadership roles in medical and healthcare technologies, global sales operations, and start-up environments, and has experience working with diverse private and public sector clients in more than 120 countries.
Jason’s passion is to grow partnerships with those who embrace the vision of a future where creating a safer environment for healthcare, commercial, academic, transportation, and residential spaces is an urgent priority.
