TOSS Seal and Cut Bands Combine Precision and Efficiency for Medical Applications
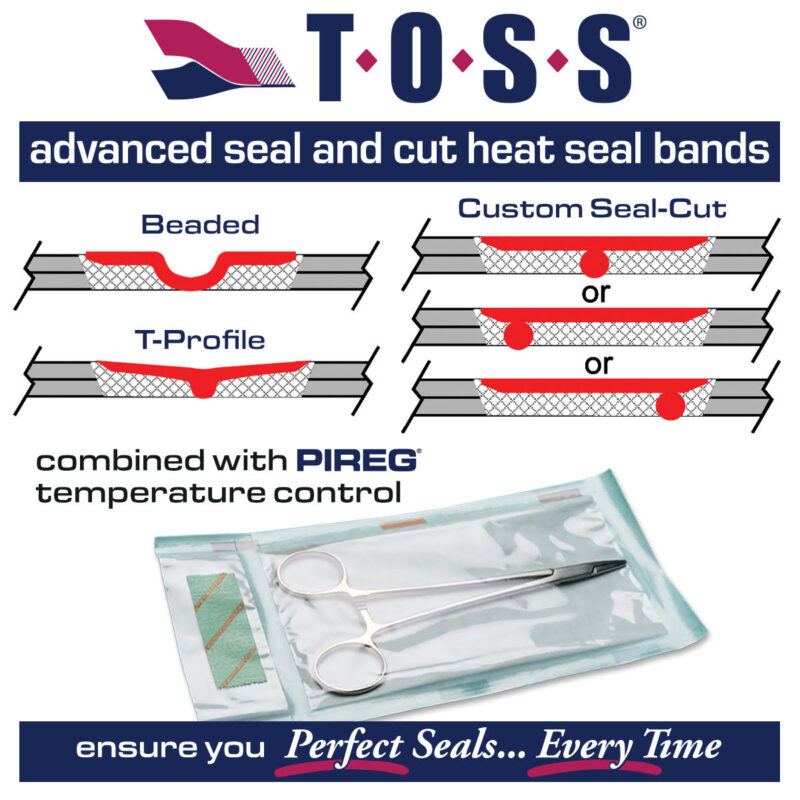
Three key offerings—Beaded Bands, T-Profile Bands, and Custom Seal-Cut (CSC) Bands—stand out for their ability to deliver consistent, reliable seals while cutting polymeric films in a single process. Each band incorporates unique design features and cutting-edge technology tailored to various applications.