It is the duty of every trained nurse, midwife, or nursing aide to make an incident report promptly about unfortunate happenings in the course of his/her duty. In fact, it is a requirement in the job description. Failure to report could cost a nurse his/her license and even face imprisonment. Yet many often do not know the right thing to do when an incident happens.
A bedside incident can be any physical or psychological injury caused by nursing that requires emergency skills, knowledge, and training of a registered nurse. It can also include any incorrect or undesirable act or omission made by a nurse.
What is an incident report? A bedside incident report is the written account of what happened either in the patient’s record, memo book, get well card, hazard communication form. It must indicate who was involved and the time it happened with the names of witnesses if there are any. Incident reports will be used by the board of nursing to investigate the case, determine who is at fault, and decide on appropriate sanctions.
Don’t know how to write an incident report? Here are 10 details to include in a bedside incident report:
1. Patient’s name and age
The patient’s name and age must be included in the incident report form because this will help you determine how to investigate the case and who has jurisdiction particularly when there is a possible criminal element. The patient’s identity should also appear in the medical record especially if it will be used as evidence in court.
2. Date, time, and place where the incident occurred
The date, time, and place where the bedside incident occurred are important details because they can establish facts about what happened. Any incident report template must include this. You may need this information to figure out how best to investigate the case or who will have jurisdiction over it. The incident’s exact location will also help you determine if there were witnesses who could be included in the investigation.
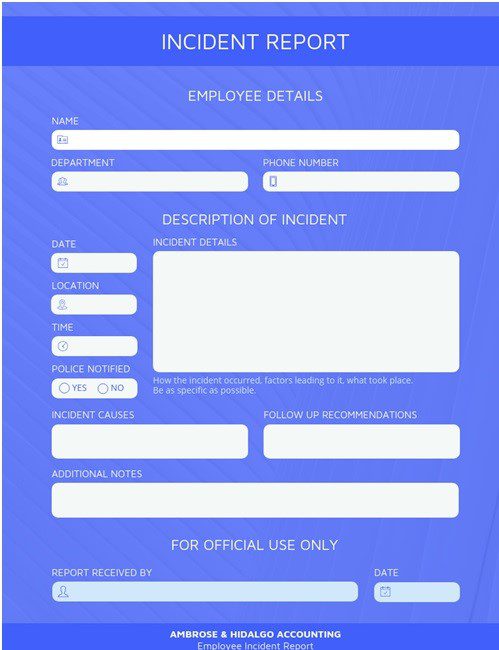
3. Description of what happened, including names of the people involved
The description should include the names of the patient and anyone closely involved in the incident. It is also helpful to include any witnesses or bystanders who may have seen what happened or who could help identify the cause of injury. The report should provide an accurate record even if the incident was not witnessed by a nurse. The written record will at least provide a consistent fact in the case.
You may consult the help of a flow chart maker if it makes your narrative more comprehensible. You can view examples of such on Venngage.
4. What steps you or your colleagues took in response to the incident, including any relevant names of nurses and doctors involved
This part of the bedside incident report is very important because it can establish what happened to prevent similar incidents from happening. It is important to list the names of nurses and doctors who were involved in responding to the incident, like those who responded to a code blue or attempted CPR.
5. Description of measures taken against possible negligence on your part
The description should include any disciplinary action that was taken against you as well as medical care you received after the incident. If you were not disciplined or given medical care, the report should say so.
6. Name of the person who prepared the bedside incident report and name of the person who approved it
This information must be included because it establishes the credibility of the written record. The signature of any person involved in reporting or investigating cases including yourself can serve as evidence.
7. Your signature and date when the event happened
Your statement must be in your own words but need not be written in the first person. It can be signed either by you or your attorney. When the patient is not physically present but you are writing about him or her, use “the patient” or “the victim.” The printed name of the witness who signed should appear.

8. Material facts that may affect the credibility of your statement
It would be helpful to include other facts that can support your written account like medical records, pictures of the scene, or samples of any drugs used when you are writing the bedside incident report. This will help establish your credibility when you defend yourself.
9. Whether or not you anticipate legal action against your nurse license and who might be responsible for such action
Your statement should include whether the legal action has been taken against your nursing license and who may be responsible for it.
10. The degree to which you can recall the events and how they happened
When should an incident report be completed? Immediately as to remember details as accurately as possible. You must describe your recollection of what occurred while being careful not to leave out any details that may be important in your defense. Details like time, place or exact statements made should be included. You cannot change or correct a statement once it has been submitted.
Conclusion
Including all of these details in a written report will help you protect yourself from being blamed for the incident. The more information you have, the better your chance of getting your license back or getting a positive result. Don’t forget that it is very important to get a good lawyer who can help you throughout the process.
