Masimo (NASDAQ: MASI) today announced the findings of a two-part retrospective study published in Telemedicine and e-Health in which Dr. Hemali Patel and colleagues at the University of Colorado and UC Health (UCH) in Aurora, Colorado evaluated the impact of remote patient monitoring (RPM) of COVID-19 patients using Masimo SafetyNet® on hospital length of stay (LOS).
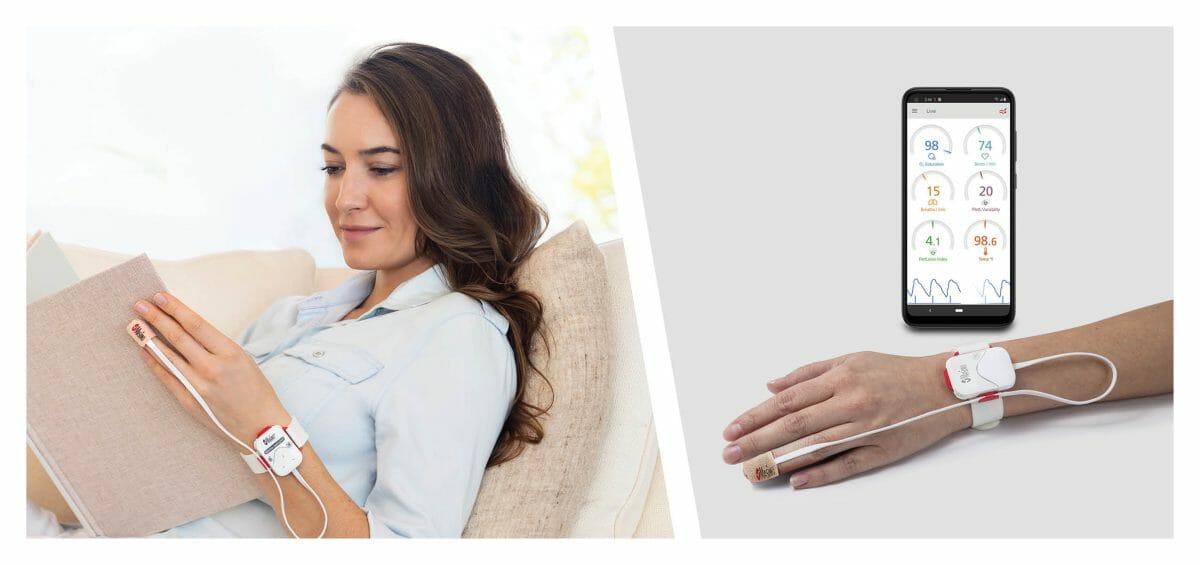
Masimo SafetyNet, a remote patient management and telehealth solution, uses tetherless Masimo Radius PPG™ SET® pulse oximetry and a smartphone app to seamlessly transmit continuous home-based patient monitoring data to hospital clinicians. The researchers found a significant association between briefer hospitalization and patients discharged with Masimo SafetyNet and without home oxygen, concluding that “Home telemonitoring after discharge for patients with COVID-19 may be a safe tool that may reduce the mean duration of hospitalization and create more bed capacity.”1
Noting the rising demand for acute care and hospital bed space during the COVID-19 pandemic, the researchers sought to evaluate whether use of a home telemonitoring system could help to optimize care—including earlier discharge from the hospital—for patients with or suspected to have COVID-19 while ensuring the “sustainability of health care capacity and resources” for those with more urgent needs, as well as decreasing usage of personal protective material, reducing pressure on personnel, and minimizing the risk of viral transmission. From March to June 2020, during the first COVID-19 surge at UCH, they implemented an RPM feasibility program with Masimo SafetyNet (study phase 1), which they redeployed during their second surge, October 2020 to February 2021 (study phase 2). Using Masimo SafetyNet with Radius PPG allowed them to remotely monitor oxygen saturation (SpO2), pulse rate, and plethysmographic respiration rate (Masimo RRp®) from a continuously staffed virtual health center, with data transmitted via Masimo’s HIPAA-compliant secure cloud service.
Retrospectively, the researchers reviewed data for all patients discharged home after an admission for COVID-19 over the two periods. Patients discharged with and without Masimo SafetyNet were compared using a two-to-one-matched case-control design, with patients matched in each time period based on age, sex, Charlson comorbidity index, and limited English proficiency. The primary outcome was hospital LOS, and secondary outcomes were a) 7-, 14-, and 30-day hospital readmission and b) return to the emergency department within 30 days. Hypothesizing that the association between LOS and use of Masimo SafetyNet might vary according to whether patients were discharged with home oxygen therapy, they also included an interaction term for the therapy in their statistical analysis. In total, they enrolled 923 patients in phase 1 (78 discharged with Masimo SafetyNet, 845 without) and 1056 patients in phase 2 (125 discharged with Masimo SafetyNet, 931 without).
The researchers found that there was a decrease in LOS for patients discharged with Masimo SafetyNet, without an increase in 30-day ED revisits or hospital readmission (from 9.1 ± 12.4 days to 7.5 ± 5.5 days in phase 1, p=0.2721; from 6.4 ± 6.4 days to 6.1 ± 5.6 days in phase 2, p=0.6913). While there was not a significant association compared to patients discharged without Masimo SafetyNet, they describe the decrease as a “trend toward an overall lower LOS.” However, as hypothesized, they observed an interaction effect between Masimo SafetyNet and home oxygen therapy: in phase 2, a decrease in LOS was strongly associated with Masimo SafetyNet patients discharged without home oxygen therapy, compared to non-Masimo SafetyNet patients—LOS decreased by an additional 36%. No other significant interactions were detected.
In their discussion, the researchers note that their study supports other work suggesting that home telemonitoring may allow for earlier hospital discharge, especially as “any reduction in length of hospitalization makes more beds available for patients.” They did not find a strong association between reduction in LOS and patients discharged with Masimo SafetyNet and with oxygen therapy, which they believe makes sense “because hypoxia portends a poorer prognosis and often a longer hospitalization.”
The authors concluded, “Our results remain relevant as we face yet more surges of admissions of patients with COVID-19. Even if the surges decrease, we face hospital capacity difficulties as we navigate ongoing COVID-19 admissions in addition to providing care for non-COVID patients. Home telemonitoring after discharge for patients with COVID-19 may be a safe tool that may reduce the mean duration of hospitalization and create more bed capacity.”
References
References
- Patel H, Hassell, A, Keniston A, Davis C. Impact of Remote Patient Monitoring on Length of Stay for Patients with COVID-19. Telemedicine and E-Health. 2022. DOI: 10.1089/tmj.2021.0510.
- Published clinical studies on pulse oximetry and the benefits of Masimo SET® can be found on our website at https://www.masimo.com. Comparative studies include independent and objective studies which are comprised of abstracts presented at scientific meetings and peer-reviewed journal articles.
- Castillo A et al. Prevention of Retinopathy of Prematurity in Preterm Infants through Changes in Clinical Practice and SpO2 Technology. Acta Paediatr. 2011 Feb;100(2):188-92.
- de-Wahl Granelli A et al. Impact of pulse oximetry screening on the detection of duct dependent congenital heart disease: a Swedish prospective screening study in 39,821 newborns. BMJ. 2009;Jan 8;338.
- Taenzer A et al. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Anesthesiology. 2010:112(2):282-287.
- Taenzer A et al. Postoperative Monitoring – The Dartmouth Experience. Anesthesia Patient Safety Foundation Newsletter. Spring-Summer 2012.
- McGrath S et al. Surveillance Monitoring Management for General Care Units: Strategy, Design, and Implementation. The Joint Commission Journal on Quality and Patient Safety. 2016 Jul;42(7):293-302.
- McGrath S et al. Inpatient Respiratory Arrest Associated With Sedative and Analgesic Medications: Impact of Continuous Monitoring on Patient Mortality and Severe Morbidity. J Patient Saf. 2020 14 Mar. DOI: 10.1097/PTS.0000000000000696.
- Estimate: Masimo data on file.
- https://health.usnews.com/health-care/best-hospitals/articles/best-hospitals-honor-roll-and-overview.