November 10, 2020
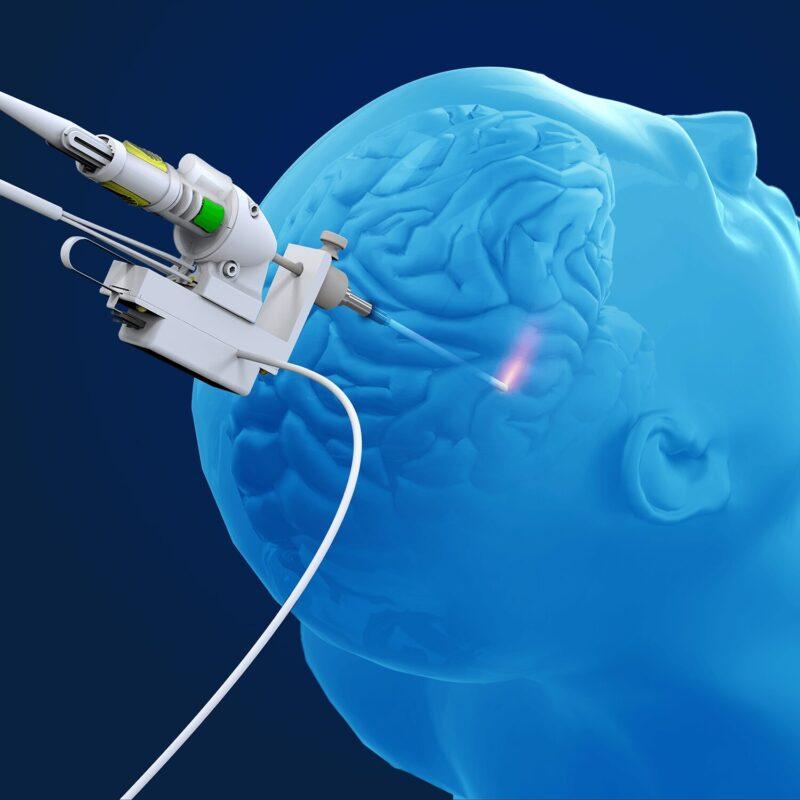
NeuroBlate System for the treatment of drug resistant epilepsy have been published in the peer-reviewed journal Epilepsy Research. The paper describes data from the LAANTERN prospective multicenter registry, sponsored by Monteris Medical. Authored by physicians at 10 leading academic medical centers, this paper is the first publication from a prospective multicenter study evaluating minimally invasive laser ablation in drug-resistant epilepsy. One year following the laser ablation procedure using NeuroBlate, the analysis of this group of 42 patients found that more than 64% were free of disabling seizures (Engel I on the Surgery Outcome Scale), with short hospitalization and minimal reported pain. While seizure freedom is the primary goal of the procedure, the study noted that more than 95% of all patients had worthwhile seizure reduction (Engel I-III). The data also showed significant improvements in patients’ quality of life (QoL).
NeuroBlate System outcome corroborates seizure freedom rates for laser ablation seen in previous cohorts,” said Dr. Patrick Landazuri, an associate professor of neurology at the University of Kansas Medical Center, epileptologist at The University of Kansas Health System in Kansas City, Kan., and the lead author of the study. “Our prospective and multicenter results suggest the outcomes are durable amongst centers and physicians who consider laser interstitial thermal therapy (LITT) a first-line surgical consideration for their patients.”
The majority of patients in this study reported an improvement in their QoL score, particularly noting reduced seizure worry and improved socialization. The paper also emphasized:
- The minimally invasive nature of the procedure with short hospital stays (median 32.7 hours)
- Minimal reported pain (median head pain score at discharge of 1.4±2.1 on a scale from 1-10 with 10 representing severe pain)
- 97% of patients discharged directly to home
“Though epilepsy surgery is a highly effective treatment for select patients with drug resistant epilepsy, it continues to be underutilized, possibly due at least in part to patient and physician concern of surgical risk,” Dr. Landazuri continued. “The availability of minimally invasive options for patients is an important step forward as suggested by our finding that 84% of patients in this study indicated to their physicians, a preference for a minimally invasive option for their epilepsy surgery.”
According to the Epilepsy Foundation, 3.4 million people in the United States have epilepsy and one third of this population lives with uncontrollable seizures that cannot be managed with pharmaceutical treatment (i.e., their condition is drug resistant). Uncontrolled seizures increase the risk for Sudden Death from Epilepsy (SUDEP) and can have other effects on a person’s physical and emotional well-being, in addition to neurocognitive development.
“We are grateful to be part of an ecosystem that includes academic researchers who are improving the lives of people with epilepsy through a procedure that demonstrates low acute surgical complication rates and short recovery times,” said Martin J. Emerson, president and chief executive officer of Monteris Medical. “More than one million people in the United States suffer from drug resistant epilepsy. Monteris remains dedicated to delivering an evidence-based surgical treatment option, through NeuroBlate, to help address the treatment gap for this population.”
LAANTERN is a post-market study designed to evaluate the performance and utilization of the NeuroBlate® System in the standard of care, “real-world” setting. This is the first prospective multicenter laser ablation study. All sites operate under an IRB-approved protocol and undergo rigorous data management and monitoring practices to ensure data quality and consistency. The registry will follow up to 1000 patients for five years, evaluating safety, quality of life (QoL), health economics and procedural outcomes including survival and seizure freedom.