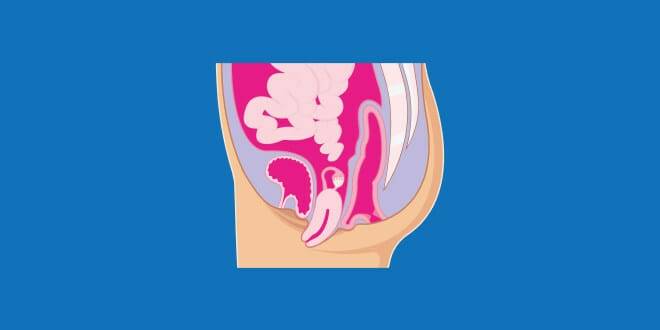
Pelvic organ prolapse (POP) is a common condition affecting over 50% of people with a uterus in their lifetime. Ligaments, fascia and pelvic floor muscles support the pelvic organs. When these support systems are compromised, one or more of the organs can shift out of position into or out of the vaginal canal. This shift can affect the bladder, rectum, uterus, urethra, or small intestines. INTIMINA’s medical expert, Margo Kwiatkowski, doctor of physical therapy shares insights into pelvic organ prolapse and treatment.
Who is at risk?
Pelvic organ prolapse affects over 50% of people with a uterus in their lifetime. INTIMINA and dr Margo Kwiatkowski explain this condition, who is at risk, and the treatment options.
Pelvic organ prolapse affects over 50% of people with a uterus in their lifetime. INTIMINA and dr Margo Kwiatkowski explain this condition, who is at risk, and the treatment options.
The support structures for the pelvic organs can be compromised by acute trauma, such as vaginal childbirth, or by long-term pressure-management issues, as seen in people with chronic constipation. The most significant risk factors for developing POP are vaginal childbirth, family history, chronic constipation, chronic cough, and higher BMI.
“Age is also identified as a risk for developing prolapse, with a higher likelihood in perimenopause and menopause. Symptoms of prolapse vary depending on the organ affected but commonly include a sensation of heaviness in the vagina, a bulge present in the vagina, urinary or faecal incontinence, incomplete bladder or bowel emptying and lower back or groin pain”, says Dr Kwiatkowski.
Treatment
Treatment options vary and depend greatly on the severity of the prolapse and its impact on the patient’s quality of life. Dr Kwiatkowski explains:
“The first line of treatment should be pelvic floor therapy with a physical or occupational therapist. These medical providers have specialised training to treat pelvic floor muscles and organ disorders. Pelvic therapy treatments for prolapse include education about proper bowel and bladder health, strategies to manage abdominal pressure correctly, and strengthening exercises. Bowel and bladder health can often be well managed with hydration, dietary changes, using a stool under the feet during bowel movements, and improved breathing strategies during defecation.
Learning how to manage intra-abdominal pressure involves improving posture, correcting lifting strategies, reducing habits of bearing down or breath-holding, and teaching proper core engagement while coughing and sneezing.
Strengthening exercises a pelvic health therapist provides will be unique to the individual’s needs. Some patients need to improve their pelvic floor strength and coordination; others need to prioritise strength in the abdominals and hips. Kegel exercises have not been shown to improve the anatomical severity of prolapse but can help with the management of symptoms, including stress incontinence.5, 6, 7, 8, 9 Isolated kegel contractions help increase pelvic floor muscle strength along with strengthening surrounding muscles to provide support for the pelvic floor further. A pelvic health therapist should thoroughly examine individuals with prolapse before beginning a pelvic floor muscle strengthening program. This is because kegel exercises are not necessary for some people with prolapse. Furthermore, it is important to have guidance on the proper performance of pelvic floor muscle contractions.
Another treatment option for pelvic organ prolapse is using a pessary. A pessary is a medical device worn inside the vagina to support the pelvic organs. Pessaries can be properly sized and managed by a urogynecologist, gynaecologist, and some pelvic health therapists. Pessaries come in various shapes and sizes to achieve the best fit and support for a person’s unique anatomy. Finding the best pessary can take a few trials. Some pessaries can be left in for months, while others need to be removed daily. Most people can learn to manage a pessary on their own at home. Pessaries are excellent long-term treatment options for those looking to avoid or prolong surgery.
Studies have demonstrated that pessaries can improve prolapse-related symptoms, pelvic floor muscular support, and potentially improve the stage or severity of the prolapse. While pessaries are specifically fitted for the individual, some over-the-counter products work similarly and may be more easily accessible. ”
Estrogen
Another treatment option for managing the symptoms of prolapse is the use of topical vaginal estrogen. “In perimenopause and menopause, estrogen significantly declines. Estrogen is responsible for many bodily functions, including vaginal blood flow and natural tissue lubrication. A similar effect happens as long as a person is lactating after childbirth. This lack of estrogen creates an environment in the vagina where prolapse symptoms are more noticeable due to dryness and a loss of tissue elasticity. Topical vaginal estrogen can be used to replenish the vaginal tissues without affecting the body as a whole. By reducing dryness and improving blood flow to the muscles and other soft tissues, prolapse symptoms can improve significantly”, says Dr Kwiatkowski.
Surgery
Surgery is another treatment option for prolapse. Surgical intervention will vary depending on many factors, including the prolapse’s severity, the patient’s age, which organs are affected, and co-morbidities such as a genetic hypermobility disorder.
Dr Kwiatkowski continues: “A person’s native tissues can be used for repair, or a surgeon may recommend using mesh to augment the tissues. The mesh used in current vaginal prolapse repairs is different than the abdominal mesh used in pelvic surgeries decades ago and no longer poses the same risks. Most surgical intervention involves elevating the organs into their anatomical position and fixating them in place. Successful surgery is determined by the patient’s satisfaction regarding symptom resolution, not simply if the anatomy has improved. Prolapse repairs can fail; some need revisions after ten to twenty successful years. A person may consider surgery if their prolapse is significantly affecting their quality of life and conservative measures have not been successful.”
“Prolapse is a common diagnosis, but it does not mean that symptoms associated with it are “normal.” Many people falsely assume that their lives must change drastically following a POP diagnosis. On the contrary, many people continue to live highly active lives with well-managed symptoms. Many younger women go on to have more children without worsening prolapse and with good recovery postpartum. The key to living a fulfilled life with prolapse is finding the best tools for your unique body. For some individuals, this means closely managing constipation and weight gain; for others, it might mean regular full-body and pelvic floor muscle strengthening. The diagnosis of prolapse does not need to interfere with a person’s quality of life, as there are excellent medical providers to help navigate the many treatment options available”, concludes Dr Kwiatkowski.