January 11, 2021
Single Use Barriers: A study described in a letter to the editor in the January issue of Mayo Clinic Proceedings entitled “Aseptic Disposable Stethoscope Barrier: Acoustically Invisible and Superior to Disposable Stethoscopes” found that aseptic disk cover barriers from AseptiScope (www.diskcover.com), previously proven to block the growth of dangerous pathogens on stethoscope diaphragms, are acoustically invisible and allow for 100% diagnostic accuracy.
In contrast, the same study reported that disposable stethoscopes were found to present an 11% misdiagnosis rate for serious clinical conditions that may have auscultatory findings such as systolic and diastolic heart murmurs.
The stethoscope commonly referred to as the clinician’s “third hand,” is the most frequently used medical instrument with over 5.5 billion annual auscultations in the US alone. The stethoscope is also a proven vector of disease transmission, with CDC cleaning guidelines that are incompatible with the intensity of stethoscope use and the high-paced workflow in clinical settings. A current approach to reduce the spread of healthcare-acquired infection (HAI) is the use of disposable stethoscopes. While the persistent risk of HAI with disposable stethoscopes has been established, this study is the first to describe the compromised performance associated with their use compared to an emerging alternative in aseptic single-use disk cover barriers.
“Failure to correctly identify auscultatory sounds 11% of the time presents a tremendous clinical and economic cost to the healthcare system,” said Sarathi Kalra, MD, MPH principal investigator of this study who is also an Assistant Professor and Research Director in the Department of Emergency Medicine at the University of South Alabama, Mobile. “Such a significant error rate creates a potential liability for health care providers who rely on accurate clinical assessments to develop appropriate, and often time-sensitive, treatment plans. The full impact of a missed diagnosis using disposable stethoscopes extends far beyond financial implications. Added morbidity and mortality from a delayed or missed diagnosis can often times lead to irreversible outcomes, especially in the acute care setting where disposable stethoscopes are frequently used,” Dr. Kalra added.
Study Design and Results
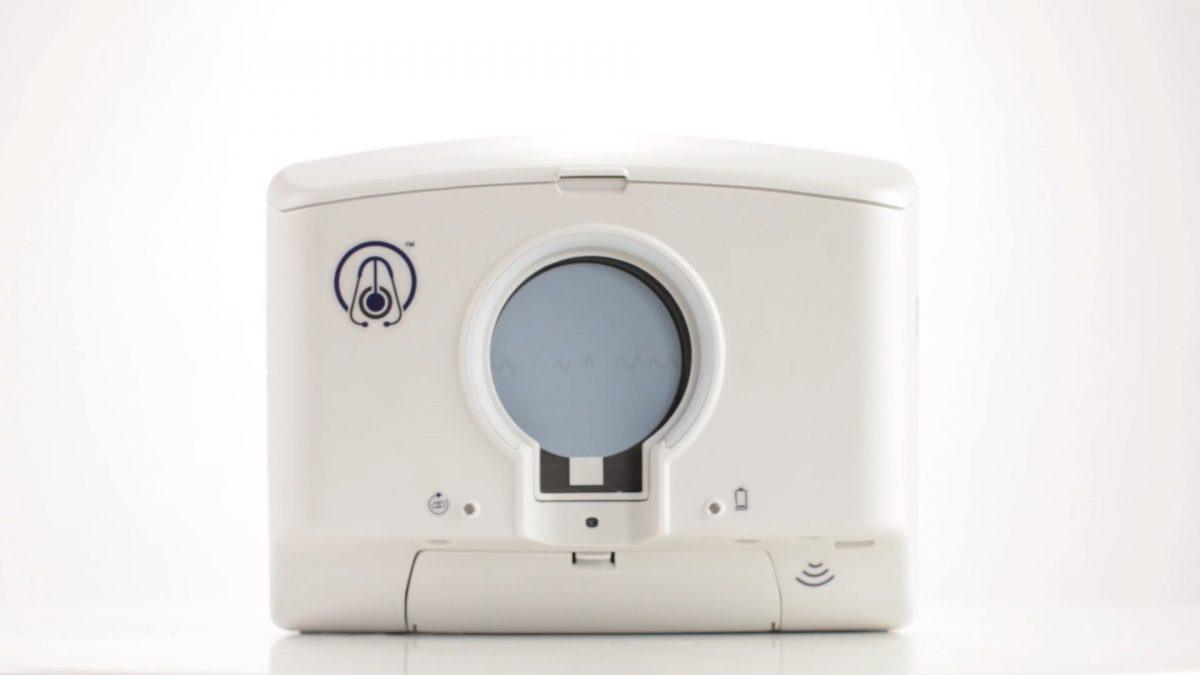
This prospective evaluation employed Littmann 3200 recording stethoscopes (3M), a simulation mannequin (iSTAN, CAE), disk cover barriers (AseptiScope), and disposable stethoscopes (Proscope 665, ADC. Inc.). Twenty-eight physicians performed auscultations in prespecified locations and listened for 15 seconds of respiratory wheezes, normal heart sounds, systolic murmurs, and diastolic murmurs. Physicians were blinded to the presence of barriers and received sounds in random order. Digital audio files were analyzed for amplitude differences (Logic Pro X, Apple Inc.), with and without a disk cover barrier in place.
Unblinded physicians then used Littmann stethoscopes with barriers and disposable stethoscopes without barriers and auscultation accuracy was recorded. The Wilcoxon rank sum test was used to compare amplitude differences among groups and McNemar’s test was used to compare diagnostic accuracy.
In 800 matched observations of Littmann stethoscopes with and without disk cover barriers, there were no differences in sound amplitude (P=1.0) across all sounds. Diagnostic accuracy of 110 auscultations using the Littmann plus disk cover barrier was 100%. The 110 auscultations with the disposable stethoscopes saw an error rate of 10.9% (12 of 110) with misinterpretation of 9 systolic murmurs as occurring during diastole and 3 diastolic murmurs identified as occurring during systole.
In subjective evaluation, 95% of physicians reported a preference for their personal stethoscope with a disk cover barrier over the disposable stethoscope.
“This important study establishes the clinical and economic advantages that our DiskCover System delivers over the use of disposable stethoscopes,” said Scott Mader, CEO, and co-founder of AseptiScope. “Our innovation allows clinicians to use their personal stethoscopes, with no loss of fidelity, to make critical clinical diagnoses accurately while protecting patients from exposure to dangerous pathogens. This study adds to an increasing body of evidence establishing The DiskCover System a clinically significant advance in the challenge of stethoscope hygiene,” Mader added.