The surgical robotics field has grown exponentially since the mid-1980s and now includes many commercially deployed systems. Furthermore, a rapidly expanding research and development community is at work to advance the capability and application space of these systems.
As healthcare practitioners become more accustomed to surgical robots, they are seeing more and more revolutionary possibilities for their application, as well as connecting with both academic researchers and industry to put their ideas into real-world practice.
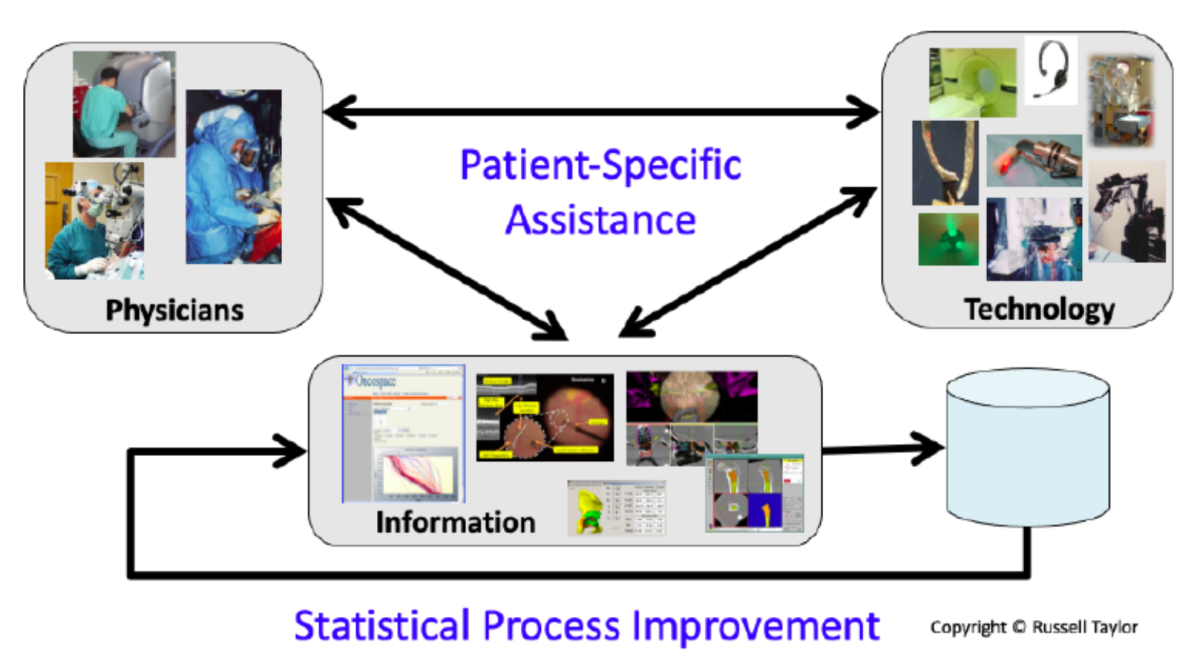
A synergistic and increasingly effective partnership has emerged among humans, technology and information to improve the safety, benefits and cost-efficiency of robotic interventions in an increasing range of surgical disciplines. The partnership also is fueling continuous improvement in surgical processes through the use of machine learning methods driven by large surgical databases.
Human-machine partnership for improving safety, efficacy and cost-efficiency of surgical robotic innovations
State of Real-World Implementation Today
As robotics acquired greater prominence across other fields (such as manufacturing) in the 1970s and ‘80s, researchers began exploring possibilities for extending computer-aided surgery into the realm of physical intervention. For example, could robotic tools offer opportunities to achieve more dependable and accurate coupling between preoperative surgical planning and surgical execution?
Starting with initial research efforts in orthopedics, stereotactic brain surgery, laparoscopic surgery and some other surgical disciplines, the pace of development since the middle 1980s has been remarkable. Surgical robots have penetrated more and more aspects of medical practice around the world. Across an expanding range of procedures, the benefits of robotic systems have been established for extending human sensor-motor capabilities in enabling extremely precise and delicate manipulation of tissue in both minimally invasive and “open” surgery. Some or all of the robot’s motions may be controlled by the surgeon, or some motions may be completely autonomous. Surgical robots can place instruments and other devices with very high accuracy relative to patient anatomy, and it is valuable, too, that the devices are mostly unaffected by ionizing radiation.
Computer-integrated systems incorporating robots can contribute to more consistent execution of surgical tasks. The technology can help ensure that an intervention is performed the same way over and over again—the benefits of which are multifold. For example, as every freshman physics major knows, better data is produced when experiments are conducted more consistently. The possibility of using large databases of information from consistently executed surgical tasks to improve surgical practice has great promise.
Patient-specific information (from images, genetics, clinical history, etc.) that is used to assist in planning and execution for individual patients can be accumulated and correlated with data on surgical outcomes for analysis via machine learning. This process can yield transformational system improvements for future patient care. The same information also can inform future surgical training. It’s a closed-loop paradigm that sometimes is described as “Surgical CAD/CAM/TQM,” emphasizing its analogy to Computer-Aided Design (CAD), Computer-Aided Manufacturing (CAM) and Total Quality Management (TQM) in manufacturing.
When most of the surgical decisions are being made dynamically and interactively during a procedure, the robotic systems tend to be more thought of as “surgical assistants.” However, there is no distinct line of demarcation between the two models. Most systems today exhibit aspects of both the Surgical CAD/CAM and assistant paradigms. And all of these systems can offer the same TQM advantages from machine learning methods using the data generated.
What’s On the Horizon?
Whereas robotic surgery systems are already being used to augment manipulation, boost distal dexterity and precision, and reduce physiological and cognitive burden of coordinated motion, other desirable attributes will be necessary to trigger wider spread commercial deployment. The next generation of technology must minimize disruption to clinical workflow, require a smaller-and-smaller physical footprint in the operating room and be flexible to system reconfigurability.
Future surgical robotics systems will harness advances in artificial intelligence, device and sensor technology, medical image analysis, systems engineering and human-machine collaboration capabilities to improve clinical care. Some areas of particular note include:
- Continuum and Soft Robots—These technologies, predicated on the need to reach deep regions of the human body safely and flexibly, are especially promising for applications requiring limited forceful interaction with the anatomy. Given their reliance on elongated and mostly rigid parts, gears and tendons, today’s tele-operated surgical systems tend to be limited in their ability to maneuver safely along sinuous paths. Emerging continuum and soft robots, however, use a combination of passive deflection (via interaction with the anatomy) and active deflection (via intentional steering), in order to circumvent obstacles. In this way, these technologies can realize complex equilibrium shapes for navigation and tissue manipulation deep in the anatomy.
- Robots for Single-Port-Access, Natural Orifice and Transluminal Surgery—Progress in development of wire-actuated mechanisms, continuum robots and catheter-like systems are enabling development of a new class of systems. Resolution of kinematic redundancy, control and unique design solutions (such as wristed instruments, snake-like robots and multi-arm foldable devices) are among the key areas of development for solutions achieving minimally invasive deep intervention and enabling new surgical access approaches.
- Precise Surgery with Image Guidance—One of the most compelling (and frequently differentiating) advantages of surgical robots is their ability to locate a tool onto an anatomic target with very high geometric accuracy. These “image-guided” surgical applications typically leverage medical images acquired either before or during the procedure for their targeting information. They usually employ a combination of medical image segmentation, interactive designation by the surgeon and (more and more frequently) automated planning methods to extract the information that they require. This information must be registered to the robot’s coordinate system, and the robot must be capable of executing the motions required of the defined task. The system sometimes is capable of utilizing additional sensing or imaging of tool-to-tissue relationships.
- System Control, Task Automation and Autonomy—Task specification and control for surgical robotic systems require answers to two basic questions: How can a human physician communicate what the robot is to do? And how can the robot, in turn, safely and reliably perform that specified task? In cases where the system simply needs to place a tool on a target identified in a medical image, move a cutter or radiation beam along a predefined path, or (in teleoperation) move a tool to mimic the motion commanded by a surgeon manipulating a control handle, these questions can be straightforward, though answering them can require sophisticated and rigorous engineering. In recent years, however, interest has increased in exploiting the potential of robotic systems to assist surgeons more actively. Tedious or repetitive subtasks can possibly be automated, and/or control can be shared between the surgeon and the robot to enhance the accuracy or the safety of the procedure. In these cases, the robot’s controller and the surgeon need a much richer shared situational awareness. Developing this shared awareness is a major subject of current research.
- Haptics and Human-Machine Interfaces—With more reliance on surgical robotic systems, the surgeon’s hands and eyes have moved further away from the scene of procedures. This trend has yielded important benefits in ergonomics, motion scaling, direct mapping of hand and tool motion, and other areas. At the same time, it also has increased the perception barrier compared to open surgery. Haptics and human-machine interfaces have been designed to help overcome this challenge. Using a variety of techniques such as force feedback and substitution of one sensory modality for another (for example, auditory cues to indicate force levels), these technologies are beneficial for reconstituting lost sensory presence. The possibilities of information-augmented displays, three-dimensional displays, augmented and virtual reality are being explored for helping surgeons to better identify surgical targets and to more accurately discern key characteristics of surgical interaction such as force and stiffness of manipulated anatomy.
- Robot-Assisted Imaging—Robotic systems can also be used to significantly assist in the process of producing images for diagnostic or interventional purposes by exploiting their ability to accurately position imaging sensors relative to patient anatomy, move sensors in precisely controlled paths or combine sensing with other forms of tissue manipulation. The capabilities can support ultrasound, X-rays, computer vision applications and other modalities.
- Microsurgery Systems—Human sensory-motor limitations can introduce severe challenges for surgical interventions on delicate structures such as the eye, ear, nerves or very small blood vessels. For example, a human hand tremor could impact a surgeon’s ability to manipulate surgical tools at the required, sub-millimetric precision. Similarly, tool-to-tissue interaction forces often fall significantly below the perceptual thresholds of human surgeons. This makes microsurgery an especially important focus of both research and commercial development around surgical robotic systems, which are proven for extremely precise, tremor-free, micron-scale motions. Magnetically manipulated microrobots, for instance, hold tremendous promise for extremely fine scale and minimally invasive interventions in the eye and other parts of the body.
Conclusion
With surgical robotic systems gaining more prevalence across applications and markets in the years ahead, patients and healthcare providers alike will become more demanding in areas such as the post-operative quality, cost-effectiveness and the unique niche that robotics technologies can offer.
The general trend in surgical care toward greater precision and earlier intervention will also produce both technical and societal challenges. Given the rapid development of imaging and diagnostic technologies and enhanced comprehension of diverse disease progressions and their impact at a system level, developers of surgical robotic systems will need to address requirements in additional areas such as:
- ability to deal with smaller and earlier lesions with even greater accuracy;
- tighter linkage of imaging, cellular and molecular biomarkers;
- system-level function for contributing to better quality of life after surgery over a longer term;
- accounting for co-morbidities in patients given increases in human longevity and lengthier survival after major illnesses, and
- contributions beyond the operating theatre and throughout a patient’s entire treatment cycle.
Ultimately, large-scale commercial uptake and clinical adoption of the next generations of surgical robots will depend on their clear and significant advantage per application relative to their cost, as well as how seamlessly they can be integrated with overall surgical workflow to contribute to better patient care.
To learn more, please see the July 2022 special issue of Proceedings of the IEEE, “Surgical Robotics and Computer-Integrated Interventional Medicine.”
