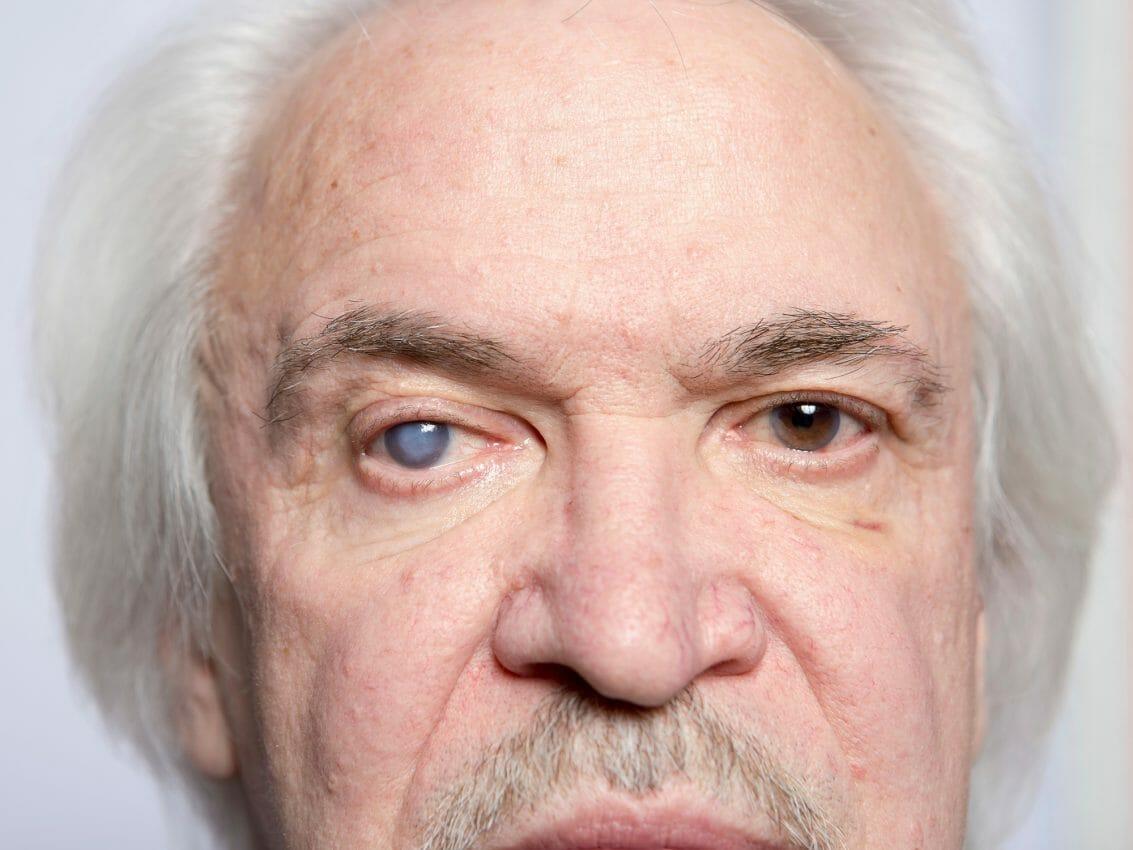
Cataracts can affect an individual’s quality of life, as they often lead to clouded vision, eye pain, difficulty seeing at night, increased sensitivity to glare, and other related symptoms. Aside from people over the age of 60, they can occur due to various factors, including aging, trauma, genetic disorders, certain medical conditions like diabetes, or excessive exposure to ultraviolet light. Unfortunately, dealing with this eye condition can be challenging as it can significantly affect your life.
Hence, if you have cataracts and are looking to address this condition, surgery offers a potential solution. However, if you’ve been diagnosed with it for the first time, it’s natural to wonder about the appropriate timing for this procedure.
Continue reading this article to learn more.
The Role Of Cataract Surgery
Cataract surgery refers to an outpatient procedure aimed at removing the clouded lens of the eye and, in most cases, replacing it with an artificial intraocular lens. It has a high success rate and is typically performed by an ophthalmologist. While this surgical idea may be daunting to some, the techniques used are well-refined, and the benefits can be significant.
By replacing the clouded lens, the procedure can restore much of the patient’s original vision. Moreover, advancements in lens technology mean that the replacement lenses used in the operation can correct other vision problems, such as nearsightedness or farsightedness, at the same time.
On the other hand, let’s look at the different surgical options available to treat cataracts. These include:
- Phacoemulsification: This is the most common type of eye procedure. It’s performed using a small incision in the cornea, through which a probe is inserted. The probe uses ultrasonic waves to break up the cloudy lens, which is removed by suction. A clear artificial lens is then inserted into the eye.
- Femtosecond Laser-Assisted Cataract Surgery (FLACS): This is another type of procedure that utilizes a laser to create an incision in the cornea and break up the cloudy lens. The rest of the procedure is similar to phacoemulsification.
- Extracapsular Cataract Extraction (ECCE): This is an older type of cataract surgery that’s not as commonly performed as phacoemulsification or FLACS. During ECCE, a larger incision is made in the cornea, and the entire cloudy lens is removed. A clear artificial lens is then inserted into the eye.
These are the different types of procedures used in treating cataracts. However, the type of surgery that’s right for you may depend on your individual circumstances and the preferences of your eye doctor. Therefore, if you have cataracts, it’s essential to consult a professional. For example, you may book an appointment with Dr Gray or other doctors in your area to get started with your recovery journey. The consultation can provide an opportunity to discuss your symptoms, concerns, and lifestyle needs. It can also enable the eye care professional to provide personalized advice and recommend potential surgical options.
Identifying The Need For Cataract Surgery
Now that you understand the role of cataract surgery, it’s time to familiarize yourself with some instances of when you should get the procedure. The answer depends largely on the impact of cataracts on your quality of life. As this condition develops slowly, there’s often no rush to have the operation until symptoms start to interfere with everyday activities.
But in general, it might be time to consider cataract surgery based on the following several key indicators:
- Changes In Vision Start Affecting Everyday Tasks: When you start having difficulties in reading, driving (especially at night), recognizing faces, or performing other activities that rely on a clear vision, surgery should be done as soon as possible.
- Adjustments To Glasses Or Contact Lenses Don’t Improve Vision: When you find that changes to your prescription lenses are no longer aiding your vision as they used to, it might be time to discuss the possibility of cataract surgery with an eye care professional.
- Glare Becomes Problematic: Cataracts can make the eyes more sensitive to light, resulting in glare. If this becomes severe enough to cause discomfort or impair vision, it might be a sign that surgical procedure should be considered.
- When You’re Of Advanced Age: As mentioned, cataracts are more common in people over the age of 60, but they can develop at any age. If you’re young and have cataracts, you may want to wait until your vision problems become more severe before considering an eye operation. But if you’re of advanced age and dealing with severe vision issues, you should consider getting one as soon as possible.
- When Your Other Medical Conditions Are Under Control: If you have other medical conditions, such as diabetes or high blood pressure, you may need to wait until these conditions are under control before having cataract surgery. This way, you can avoid more serious health complications that may arise during and after the procedure.
By keeping these instances in mind, you’ll have an idea when should be the right time to get cataract surgery. However, it’s crucial to know that the decision of when to get this medical intervention is a personal one. There’s no one-size-fits-all answer, as the best time for the procedure may vary depending on your individual circumstances.
Preparation For Cataract Surgery
After understanding the scenarios that warrant cataract surgery, it’s important to understand the preparation process associated with the procedure. Generally, the preparation for this medical intervention may involve several steps. For instance, you’ll be required to undergo a preoperative assessment, which may include detailed measurements of the eye, a review of your medical history, and a discussion about the best lens for cataract surgery, determining which type of lens would be most appropriate for your individual needs.
The doctor will also provide instructions on medications; in some cases, you may be asked to temporarily stop or adjust the dosage of certain medicines to avoid adverse side effects.
The Procedure And Aftercare
Once you’ve gone through all the necessary preparations, you can proceed to learn the surgery and the aftercare involved. Typically, the surgery takes about an hour and is performed under local anesthesia. After the operation, you’ll likely need to wear a protective shield over your eye for a few days and use prescribed drops to prevent infection and control inflammation.
Regular follow-ups will be necessary to monitor the healing process. Full recovery often takes a few weeks, but many patients report noticeable improvements in their vision within a few days of the procedure.
Conclusion
Cataract surgery is a well-established procedure that can offer significant improvements in vision and quality of life. However, the decision to undergo this medical intervention shouldn’t be made lightly. Therefore, if you’ve been diagnosed with cataracts, keep the information mentioned above in mind to help you make an informed decision about when to get cataract surgery.