Bariatric Surgery: Obesity, characterized by excessive body fat accumulation, poses severe health risks such as heart disease, diabetes, and hypertension. It often results from genetic, behavioral, and environmental factors, which can lead to the need for surgical intervention when lifestyle changes prove insufficient.
According to the CDC, obesity is found in 2 out of 5 individuals in the US. It is quite prevalent in adults and is an expensive chronic disease. Bariatric surgery offers a range of options to battle obesity and its related conditions.
In this article, we will study the different types of bariatric surgeries and evaluate their effectiveness in achieving long-term weight loss goals.
Types of Bariatric Surgery
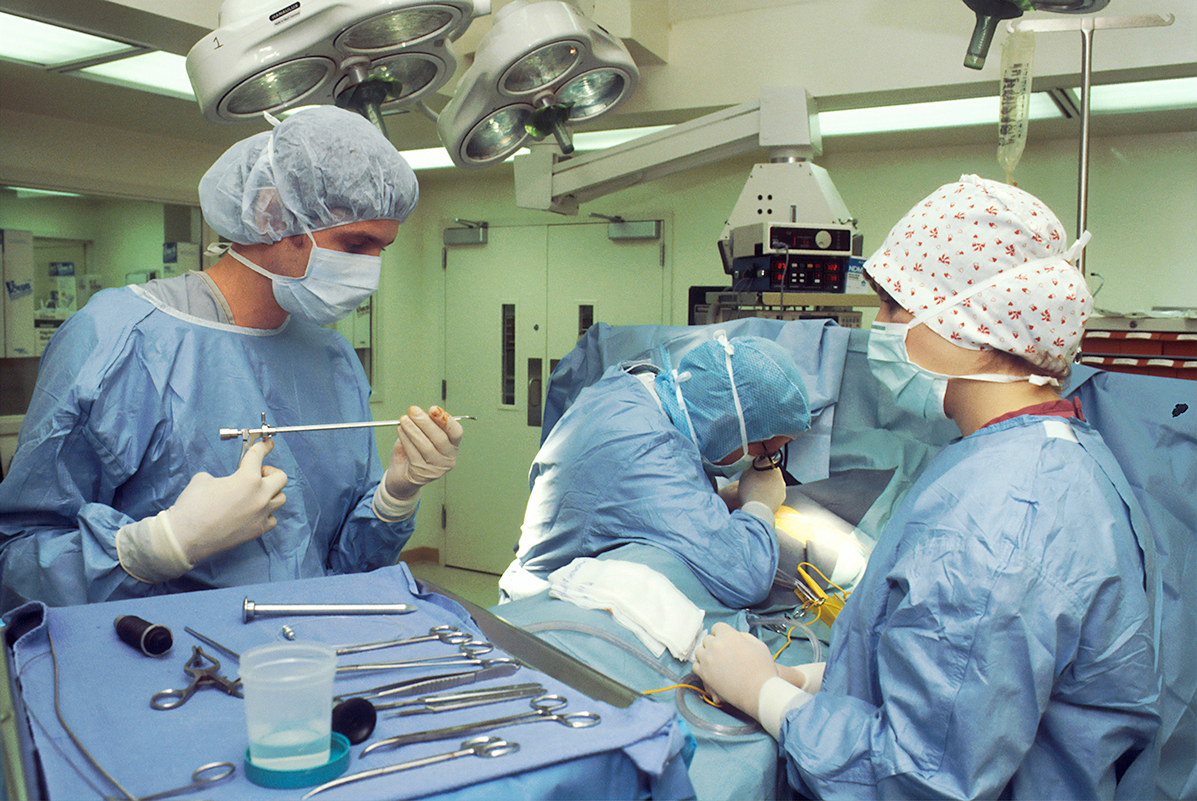
This surgery encloses several types of procedures aimed at promoting significant weight loss by adjusting the digestive system. According to ScienceDirect, 280,000 bariatric procedures were executed in 2022 in the US. This was a 6.5% increase from the number of procedures done in 2021. Bariatric surgery is of different kinds and is tailored to meet individual health necessities and weight loss objectives.
The most standard types include gastric bypass, sleeve gastrectomy, and adjustable gastric banding, each with an approach to reducing food input or nutrient absorption.
Gastric Bypass
Commonly referred to as Roux-en-Y gastric bypass, this widely used bariatric procedure involves forming a small stomach pouch and redirecting the small intestine. During the procedure, a surgeon divides the stomach into two sections, leaving a tiny pouch that limits food intake.
The small intestine is then joined to this pouch, bypassing most of the stomach and upper intestine, which lessens calorie absorption. Candidates should know that this procedure results in rapid weight loss and requires lifelong changes to diet and supplements.
Common deficiencies that might occur after a gastric bypass include vitamin B12, thiamine, iron, folate, zinc, and vitamin D. According to the National Library of Medicine, rapid weight loss might also increase the probability of stone formation in the gallbladder. It might occur in 30% of patients. Regular follow-ups to prevent nutrient deficiencies and ensure long-term success.
Sleeve Gastrectomy
Sleeve gastrectomy, more commonly known as gastric sleeve surgery, implicates removing approximately 75-80% of the belly, leaving a narrow tube-like structure. This remarkably reduces the gut volume, limiting food intake and reducing the production of ghrelin, the appetite hormone.
According to the Cleveland Clinic, around 150,000 sleeve gastrectomy procedures are performed every year in the U.S., and 380,000 procedures globally. The patient can lose up to 25 to 30% of their body weight after the surgery. This weight loss can be sustained for up to 5 years if proper commitment to long-term dietary changes and regular medical follow-ups are done.
Unlike gastric bypass, nutrient absorption is not significantly affected, but patients must follow strict nutritional guidelines to avoid vitamin deficiencies and regain optimal health.
Adjustable Gastric Band (Lap-Band)
In this surgery, a silicone band is wrapped around the upper portion of the gut. This creates a small stomach bag that limits food consumption, making patients feel full with less food. The band can be tensed or relieved by injecting saline into a port under the skin, allowing adjustments based on weight loss progress.
Candidates should know that while the procedure is reversible and adjustable, it typically results in slower weight loss than other surgeries. Regular follow-ups are necessary to ensure the band is properly adjusted and functioning effectively.
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
The procedure involves cutting a portion of the gut, just like sleeve gastrectomy, and rerouting a considerable section of the small intestine. This surgery results in substantial weight loss but also carries higher risks of complications and nutrient deficiencies.
Candidates must commit to lifelong supplementation and routine medical monitoring. BPD/DS is normally reserved for candidates with severe obesity or those who haven’t achieved results in other weight loss techniques. It offers long-term success but requires strict follow-up care.
Comparative Effectiveness of Bariatric Surgeries
The effectiveness of bariatric surgeries varies depending on the type and particular patient factors. Gastric bypass typically results in rapid and significant weight loss, often 60-70% of excess weight, with long-term success in managing obesity-related conditions. Sleeve gastrectomy offers similar outcomes, though weight loss may be slightly slower.
The adjustable gastric band produces more gradual results but is less invasive and reversible. BPD/DS leads to the greatest weight loss but carries the highest risk of complications. Ultimately, the most effective procedure depends on a patient’s health, lifestyle, and commitment to post-surgery care and dietary changes.
Factors to Evaluate When Choosing a Bariatric Surgery
When choosing a bariatric surgery, several factors must be carefully evaluated. The patient’s overall fitness, weight loss objectives, and any underlying medical ailments play a critical role in determining the most suitable procedure. Lifestyle factors, such as the power to commit to long-term dietary modifications and regular follow-up care, are also crucial.
Additionally, the potential risks and benefits of each surgery should be weighed, as some procedures are more invasive or have higher complication rates. It’s also essential to consider the financial aspect, including insurance coverage and the bariatric surgery cost, which can vary significantly depending on the procedure.
According to the Bariatric & Metabolic Center of Colorado, the average cost of a bariatric surgery can vary between $14,000 to $23,000. However, the cost will vary according to the type of procedure you are choosing. You must consider every aspect before finalizing the cost and also ask for any hidden charges.
Expert Opinions and Patient Testimonials
Expert opinions and patient testimonials provide a valuable understanding of the success and challenges of bariatric surgeries. Surgeons often emphasize the importance of individualized treatment plans. They know that the best results come from carefully matching the procedure to a patient’s health and lifestyle.
Patients who have undergone these surgeries often share their experiences of significant weight loss, improved health, and enhanced quality of life.
A study found that all-cause mortality was 16% lower in people who had undergone bariatric surgery than those who had not. Furthermore, the death rates for individuals who had weight loss surgery decreased by 29% for cardiovascular disease and 43% for cancer. Additionally, the mortality rate for diabetes dropped by 72% compared to those who did not undergo the surgery.
Frequently Asked Questions
What are the key metrics used to compare the effectiveness of different bariatric surgeries?
Key metrics used to compare the effectiveness of different bariatric surgeries mainly include the percentage of excess weight loss (EWL). It also compares the progress or resolution of obesity-related health disorders (like diabetes or hypertension) and the long-term sustainability of weight loss. Patient satisfaction, complication rates, and recovery time also play critical roles in assessing the success of each procedure.
What personal health factors should be considered when choosing a bariatric procedure?
Personal health factors like body mass index (BMI), the presence of obesity-related conditions (like diabetes), and previous weight loss attempts should be considered. Additionally, a patient’s ability to adhere to long-term dietary changes, their medical history, and the risk of surgical complications are also essential to consider.
How do lifestyle and personal goals impact the choice of bariatric surgery?
Lifestyle and personal goals significantly impact the choice of bariatric surgery. Different procedures require varying levels of commitment to long-term dietary changes, physical activity, and follow-up care. Personal goals, such as the desire for gradual weight loss or reversible procedures, also influence the decision-making process.
Choosing the Right Bariatric Surgery
Selecting the most effective bariatric surgery depends on individual health needs, lifestyle factors, and long-term goals. Each procedure offers unique benefits, but success requires a commitment to post-surgery care and lifestyle changes. By consulting with healthcare professionals and considering key factors, patients can make informed decisions and achieve lasting weight loss and health improvements.